Rotator cuff arthropathy is a sequential, progressive process of glenohumeral joint degenerative changes associated with chronic rotator cuff tears.
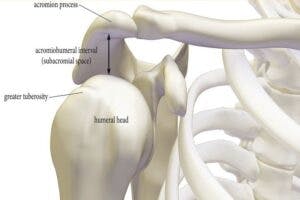
Rotator cuff tear arthropathy represents shoulder pathology characterized by rotator cuff insufficiency, decreased acromiohumeral intervals, and arthritic changes of the glenohumeral joint.

Often, in the presence of chronic rotator cuff tears, there is a superior migration of the humeral head, erosion of the greater tuberosity, and the humeral head structural changes resulting in features similar to the femoral head (known as femoralization).
In addition, there are changes of the coracoacromial arch causing it to have a similar structure to the acetabulum of the hip joint (known as acetabularization).
These structural changes can result in the narrowing of the acromiohumeral interval (AHI) and the development of glenohumeral joint arthritis.
DIAGNOSIS
Patient’s history and radiography are used to diagnosis arthroplasty. Diagnosis can be confirmed with shoulder x-rays showing glenohumeral arthritis with a decreased acromiohumeral interval.


Biomechanical Structural Destruction
A massive rotator cuff tear leads to mechanical unloading of the rotator cuff. This lack of normal stress impacts homeostasis and damages tissue at a cellular level. With these changes, there is a loss of humeral head compression which contributes to loss of humeral head centralization and a change in the location of the fulcrum of the glenohumeral joint.
With rotator cuff insufficiency, the humeral head translates superiorly and anteriorly as the patient lifts their arm. This translation causes breakdown of the cartilage and bone and allows the release of enzymes that damage the surrounding tissues. With the loss of an enclosed joint capsule, there is a leak of capsular fluids outside of the joint which effects the joint surfaces and can contribute to atrophy of the cartilage. Accompanying pain and loss of range of motion leads to further deterioration of the joint and supportive soft tissues.
Conservative Treatment
Nonsurgical management is the first line of treatment in most patients. This will include modification of provocative activities, subacromial steroid injections, and physical therapy.
Physical therapy should be focused on correcting modifiable physical dysfunctions, not at treating the pathology. Goals aimed at restoring full, pain-free range of motion, muscle flexibility, joint mobility, optimal postural alignment, correcting muscle imbalances, and improving proprioception are addressed.
Patient education is a crucial component, including avoiding provocative and aggravating activities. Exercises to facilitate, improve and maintain range of motion and optimal motor control are necessary to limit progression and further damage.
A comprehensive home exercise program should be prescribed to assure range of motion and proper mechanics are maintained beyond the episode of care.